Back to Basics – What is a Biofilm and How is it Formed?
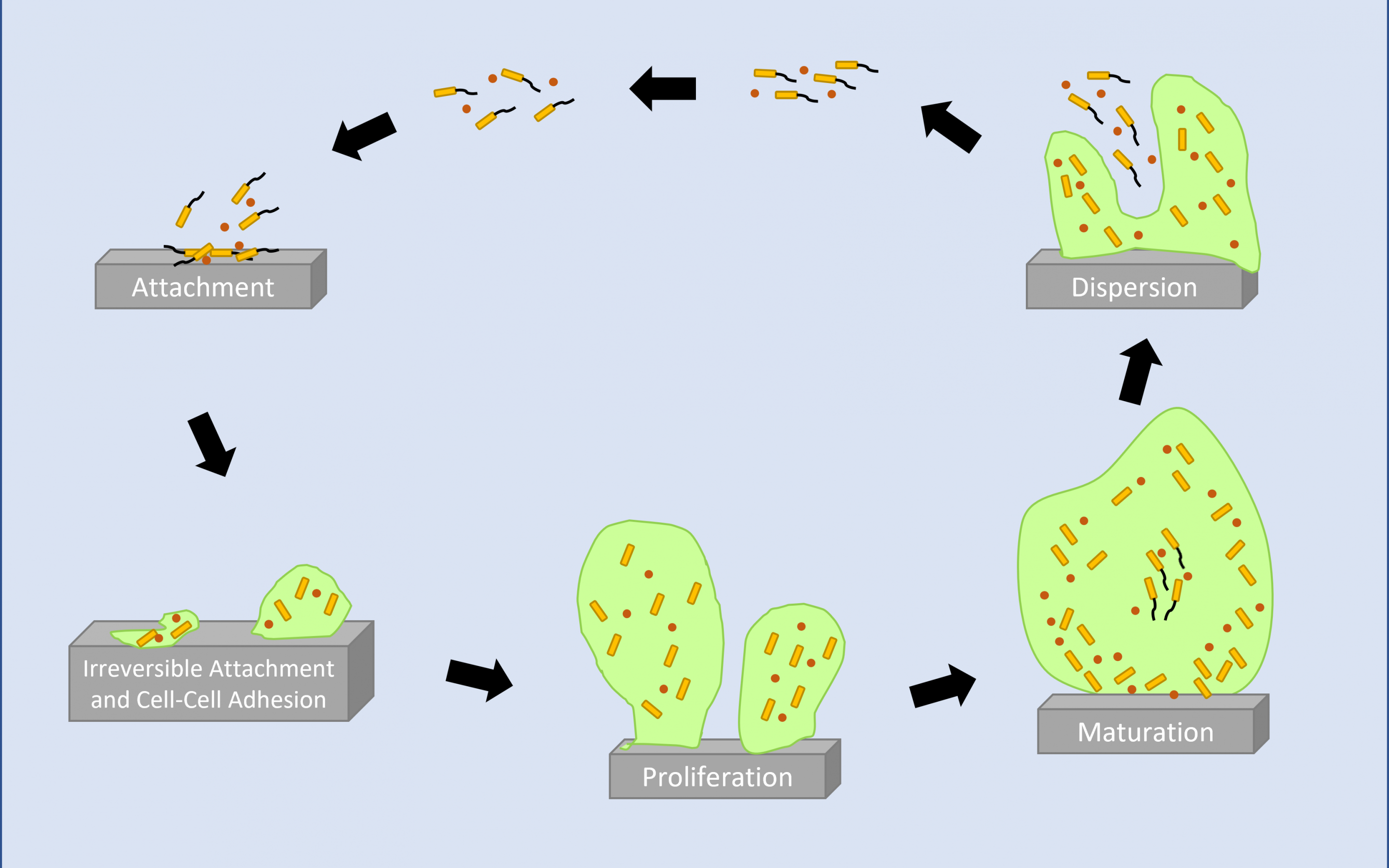
In the simplest terms, biofilms are formed when microorganisms, such as bacteria, yeast and fungi attach and proliferate on a surface. Once attached the microorganisms form and reside within a self-produced matrix structure. Biofilm has a self-perpetuating lifecycle. The first stage is Planktonic (free-living) microorganisms attached to a surface. This could be a solid surface such as a catheter, or a tissue surface such as a wound. The surface-attached planktonic bacteria begin to aggregate and secrete a protective matrix (exopolymeric substance, EPS). Over a period of hours and days, the community proliferates and mature biofilms can house single and mixed microbial species. Mature biofilm bacteria shed planktonic cells or fragments of themselves which colonise adjacent surfaces to form new communities.
Where Are They Found?
The bacterial cells’ existence is a naturally occurring process whereby bacteria are able to protect themselves from environmental challenges such as temperature fluctuations, desiccation, antibiotics, antiseptics, and immune cells. Not all are disease-causing, for example, microscopic biofilms formed around hair follicles form part of the body’s protection from invading disease-causing organisms. Another common example of these naturally occurring films is dental plaque.
Impact on Human Health
Bacterial biofilms can create a particular problem for human health with approximately 80% of chronic and recurrent microbial infections in the human body being due to bacterial biofilm.1 Mammalian infections include chronic wounds, ear infections, urinary tract infections and lung infections commonly seen in cystic fibrosis patients.
Biofilms and the Ageing Population
The prevalence and challenges associated with biofilm research in healthcare is accelerated due to the increasing aging population. Currently, 566 million people are 65 years old worldwide, with estimates of nearly 1.5 billion by 2050, particularly in developing countries.
If pathogenic bacteria entering our body are not rapidly inactivated by our immune system, they can form microbial biofilms which may trigger an infection. Biofilm infections are characterised as being persistent and recurrent, leading to chronic conditions that are extremely debilitating to those suffering from such infections.
In addition to causing chronic infections, environmental biofilm is prevalent in healthcare facilities, particularly in moist areas such as drains, sinks, toilets and showers. The bacteria can tolerate disinfection and the biofilm matrix also provides an ideal environment for the transfer of antibiotic resistance between bacteria, which exacerbates the significant problems associated with antibiotic-resistant bacteria in healthcare facilities.
Water Systems and Food Production
Microbial contamination in water systems is a global problem that spans numerous industries. Water distribution systems are susceptible to biofilm formation which can affect water quality and food production. It can also cause corrosion of cast iron pipes contributing to the aging of our water infrastructure. The organisms and their products may decrease disinfectant levels (by increasing disinfectant demand), pose a direct public health risk, and create taste and odour problems.
Microbial contamination in water treatment plants can be a health risk. These bacterial growths will naturally form and can be difficult to remove from tubes, pipes and water tanks. Biofilm grows on the hulls of ships costs the shipping industry billions of dollars per year. Multiple layers of these bacteria increase the drag force significantly, leading to increased fuel shipping costs.
How to Test Antibacterial Products Against Bacterial Biofilms
As we learn more about the role of biofilms and the significant challenges that healthcare-associated and environmental they can create, we can begin to look at more effective ways to control the microorganisms. New devices are emerging that are designed to better manage them, and new approaches and test methods are required to assess the efficacy of anti-biofilm technologies and devices.
Perfectus Biomed’s mission is to harness innovative science to improve lives. We endeavour to use our knowledge, expertise, and capabilities to provide best-in-class scientific services to test products and technologies across Medtech and Biopharma industries. We test products under the conditions in which they are intended to be used, within environments they will encounter. Perfectus Biomed will work with you to help you understand the benefits of different biofilm testing models and to help you to choose the most suitable method for your product.
Perfectus Biomed are a leading global provider of GLP-compliant, ISO 17025 accredited biofilm models and have experience across a number of sectors including oral biofilms, wound care, medical devices, and industrial biofilms. Test methods range from high throughput screens to complex tissue models designed to mimic ‘real-world situations’ in order to assess antimicrobial products designed to address the prevention and removal of biofilms. Our ex vivo tissue models also test for lung biofilm (cystic fibrosis) models as well as urogenital infections (STIs and UTIs)
For more information about the types of biofilm testing Perfectus Biomed can offer contact our experts at info@perfectusbiomed.com or call +44 (0) 1925 737237.
References
1. Khan A. U., and Misba L., Sharma D. (2019) Antibiotics versus biofilm: an emerging battleground in microbial communities
2. Kline A. K., and Bowdish, D. ME. (2016) Infection in an aging population. Current Opinion in Microbiology 2016, 29:63–67